Nina Notman reveals how breast milk research is inspiring a new generation of infant formulas and opening the door to therapeutic advances
The World Health Organization (WHO) recommends that babies are exclusively breastfed for the first six months of their lives. In 2010, when I was pregnant with our first child, the ‘breast is best’ message was drummed into us at antenatal classes. Besides, our mothers had breastfed us, all our friends and family had breastfed their children, I was always going to breastfeed our children. Or so we thought.
What we didn’t know before the birth is that my body – for some undetermined reason – doesn’t produce milk. Nothing. Our children were fed infant formula – just like millions of other babies whose parents do not breastfeed either through choice or necessity.
If we’d actively chosen to formula feed, I imagine there would have been a careful pre-birth selection process. In the event, the formula product our children drank was chosen in a panic: an urgent, sleep-deprived blind choice between the brands on offer in the fridge of the paediatric ward. We never got around to changing it.
Most formulas are based on cows’ milk with modifications and supplementations to make it more suitable for the human baby. Ingredients vary between brands and products, and formulations are constantly evolving as our understanding of what infants need to thrive grows and scientific advances open the door to novel ingredients.
One spoon or two
The medical and public health communities unanimously agree that breast milk is the optimum food for babies. It’s therefore to be expected that the composition of infant formula is slowly edging closer to that of breast milk. The biggest change in infant formula in recent years has been the addition of human milk oligosaccharides (HMOs).
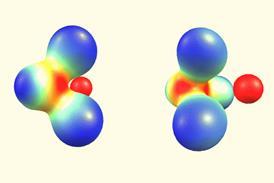
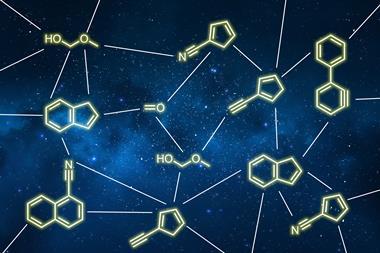
First identified in breast milk in the 1930s, HMOs are the third largest solid component of human milk and are the key differentiator between it and that of the cow. ‘They are about 300 times more concentrated in human milk when compared to the oligosaccharides in cow’s milk,’ says Lay Kwan Goh, a spokesperson for BASF. This multinational chemical giant manufactures the HMO 2′-fucosyllactose (2′-FL) for use in infant formula. HMOs are also much more structurally varied than their bovine counterparts, with more than 150 different HMOs identified so far in human milk.
HMOs are not digestible, so their role isn’t solely to feed infants. Instead, the scientific consensus is that these molecules support the immune system, both in the gut and throughout the rest of the body. But details of how remain extremely sketchy. ‘We’re just at the tip of the iceberg when it comes to understanding their wide range of potential benefits,’ a Nestlé spokesperson told Chemistry World. Nestlé is a multinational food and drink conglomerate that manufactures infant formula brands that include HMO-containing NAN.
For the body to bother to produce more than 150 distinctive HMO molecules, it’s reasonable to assume that they each serve a unique biological purpose. To fully unpack the biological function of HMOs, scientists must therefore study each compound separately. Yet the biological function of only a handful of HMOs has been studied in detail, explains Lars Bode, a HMO researcher at the University of California San Diego in the US. ‘Even for these the full story remains elusive’, he adds. For more on the challenges of fundamental HMO research see box Sugar chemistry below.
Sugar chemistry
In the approximately 90 years since they were first identified, scientists have pinpointed and determined the structure of more than 150 unique human milk oligosaccharides (HMOs) in breast milk. These are not present in equal proportions. ‘50% of the mass of HMOs in milk is represented by less than 20 structures,’ explains Steven Townsend, a chemist and HMO expert at Vanderbilt University in Tennessee, US.
To study their individual biological functions, scientists need to be able to get their hands on enough of each molecule. This remains a significant challenge. ‘The major reason the functioning of individual species of HMOs is still not clear is due to the lack of access to the pure compounds in sufficient amount,’ says Xi Chen a chemist and HMO expert at the University of California, Davis, US.
An HMO mixture can be easily extracted from breast milk. But due to their similar structures and physical properties, it’s not possible to then separate out its more than 150 different components, explains Townsend.
For any HMOs destined for commercialisation, the genetic modification of bacteria or yeast to enable them to produce the respective HMOs is the most economic option. For smaller scale research purposes, chemical or enzymatic synthesis can work. Due to their complex structures, HMOs can be extremely challenging to synthesise.
The entire synthesis will be done with the press of a button
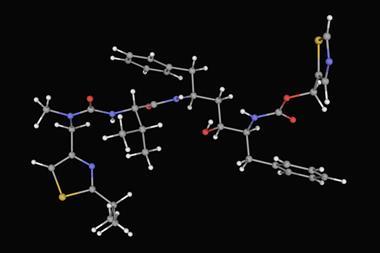
Townsend’s group uses chemical synthesis. ‘We made one of the simplest HMO compounds in human milk and it took us close to two years to make it,’ he explains. In an attempt to speed things up, Alexei Demchenko, a carbohydrate chemist from Saint Louis University, Missouri, US, is in the early stages of developing an automated HMO chemical synthesiser.
‘Our target is to synthesise all the core structures of human milk oligosaccharides,’ says Demchenko. His synthesiser is a homemade platform built from a high-performance liquid chromatography (HPLC) instrument that is normally used for compound separation. At the start of the experiment, the HPLC autosampler is loaded up with the required monosaccharides and reagents. ‘The entire synthesis will be done with the press of a button,’ Demchenko explains. So far, his group have completed one successful synthesis using their instrument and are currently tweaking the process to boost the yield produced.
For chemical synthesis of HMOs, it is the complex protecting and deprotecting strategies that cause the biggest bottle necks. Enzymatic synthesis doesn’t have this issue, explains Chen. ‘With enzymes, you don’t need to protect anything, just put things together and they will form the linkage that you desire as long as you choose the right glycosyltransferase.’
So far, Chen’s group has synthesised around 50 different HMOs using enzymes. These are all molecules with linear core structures; HMOs with branched core structures still evade her. ‘If we identify a good beta-1,6-N-acetylglucosaminyltransferase then, in principle, we can make all of the human milk oligosaccharides,’ she says.
Fermenting the future
Infant formulas containing HMOs started to be launched in 2015 and for pragmatic reasons most brands currently contain just two of these oligosaccharides: 2′-FL and lacto-N-neotetraose. Both are easy to mass manufacture using fermentation and have been proven as safe and effective in growth trials.
But in academic circles, some controversy surrounds the addition of 2′-FL to formula – as it isn’t universally present in all breast milk. ‘About 20% of the moms don’t make any of it,’ says Bode. The worry is that nature’s occasional omission of 2′-FL might not be by accident, and that this might indicate that it is not a molecule that is beneficial for all infants to be fed. There is still plenty of fundamental research that needs to be done here, Bode says.
Industry, meanwhile, is charging ahead with the addition of HMOs to formula, with more complex combinations on the near horizon. The Danish bioscience company Chr. Hansen, for example, has developed a five component HMO mixture containing 2′-FL, 3-fucosyllactose, lacto-N-tetraose, 3′-sialyllactose and 6′-sialyllactose. Like BASF, Chr. Hansen manufacturers ingredients for infant formula rather than formula itself.
‘The results of our scientific studies in infants shows that the mixture of five HMOs positively influence digestion by improving stool consistency and stool frequency. The stool pattern resembles that of breastfed infants,’ says Katja Parschat, head of HMO research and development at Chr. Hansen. Further scientific data from a trial using the HMOs at concentrations comparable with breast milk is expected soon, she adds.
As knowledge of HMOs – both of their structures and biological functions – has blossomed, so have the aspirations for these molecules beyond infant formula. They are already sold as prebiotic supplements for all age groups, and researchers are starting to explore broader applications for them. See box HMOs beyond formula below for more details.
HMOs beyond formula
The main role for manufactured human milk oligosaccharides (HMOs) is in infant formula. Their secondary use as off-the-shelf prebiotics for all age groups was perhaps an inevitable follow-up act. But – as researchers are now finding out – the potential uses for these biologically-active molecules is much vaster than was initially predicted.
Lars Bode, at the University of California, San Diego, US, is leading the hunt to identify novel medical applications for HMOs. The main disease he is working on is necrotising enterocolitis, a serious newborn gastrointestinal problem that is known to affect many more formula-fed infants than their breastfed equivalents. His group is developing the use of the the HMO disialyllacto-N-tetraose as a therapeutic for babies identified at being at risk of developing the condition.
Specific HMOs can be used to treat diseases like heart attack and strokes
Bode is also part of a University of California, San Diego, collaboration developing a point-of-care diagnostic to measure the quantities of disialyllacto-N-tetraose in breast milk. ‘If we measure these protective oligosaccharides in mom’s own milk, or in donor milk products, then we can identify suitable batches to feed a preterm infant [at risk of developing the disease],’ Bode says.
Bode and his collaborators are in the earlier stages of exploring the use of HMOs to treat and prevent adult diseases involving chronic inflammation. ‘We’ve shown in animals that specific HMOs can be used to treat diseases like heart attack and strokes,’ he says. But this is just the beginning, Bode adds. ‘As we get a deep mechanistic understanding of what all these oligosaccharides do on a cellular molecular level [during breastfeeding], this will then allow us to develop new therapeutics based on those components for people of all other age groups as well as babies.’
Brewing up proteins
While formula companies remain focused on the carbohydrate composition as a means to push their formula milk closer to that produced by nature, two start-up companies are tackling the humanisation of another major component of breast milk: the proteins.
Singapore-based TurtleTree is starting with lactoferrin, a protein that is highly abundant in breast milk and has known antimicrobial properties. Lactoferrin is also naturally present in cows’ milk, although with a subtly different structure and at significantly lower concentrations. Supplementary bovine lactoferrin extracted from cow’s milk has been added to infant formulas since the 1980s.
We’re able to recreate the proteins found in human milk
TurtleTree uses precision fermentation to manufacture lactoferrin. It is ‘cultivated using microorganisms in a bioreactor’, according to Jess Nguyen, business manager at TurtleTree. ‘These host cells multiply at a fast rate just like the beer brewing process, using relatively low-cost growth nutrients, and secrete out the target protein which is then purified and is very close to the protein from human milk itself,’ says Nguyen.
The lactoferrin launch is planned for mid- to late-2022, says Nguyen, adding that manufacturing is currently ramping up and scientific testing is underway for regulatory approval. Bovine lactoferrin is also sold as an immune-boosting supplement for adults, and TurtleTree plans to target this market with its product too.
Helaina, a start-up company based in New York, US, is looking to produce human-identical proteins for inclusion in infant formula. It is also using precision fermentation. ‘We have a microbial expression platform that we’ve developed in-house,’ says Helaina’s founder Laura Katz. ‘We’re able to recreate the proteins found in human milk that are identical in sequence and in post-translational modifications similar to what’s found in human milk.’
Helaina hasn’t yet announced the proteins it plans to commercialise first nor disclosed any timelines to market. But – as for TurtleTree – the plan is far bigger than just making a humanised protein or two. Eventually, Katz wants Helaina to reproduce every major component of human milk separately in the lab and then mix them together to form a human milk formula.
Cell-cultured human milk
TurtleTree is also aiming to manufacture a complete human milk product, but using a very different tool set. The plan is to persuade human cells to produce human milk in a bioreactor: cell-cultured human milk.
We can make milk outside the body if we can grow the cells in the right way
Another start-up is also simultaneously attempting the same quest. Leila Strickland, a cofounder of Biomilq, says she dreamt up the idea of cell-cultured human milk in 2009 while struggling to breastfeed her son. A postdoc in cell biology at the time, she jumped into trying to understand the biological reasons for the challenges she was facing. ‘The thought just came to me that we can make milk outside the body if we can grow the cells in the right way,’ Strickland says.
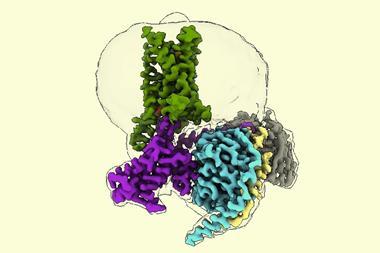
Mammary epithelial cells are at the heart of both the Biomilq and TurtleTree process. In nature, these cells reside in layers in the breast tissue where they produce milk on instruction from hormonal messengers. They absorb nutrients from the blood stream on one side of the layer and secrete milk out the other side, into mammary gland modules. Similar happens in the bioreactors. The cells arrange themselves in a layer, nutrients are absorbed from the cell culture media beneath the cells and human milk flows out above.
Strickland is clear that the milk produced in bioreactors is not breast milk. ‘It won’t ever reproduce all the same qualities and features of breast milk,’ she says. Its composition is, however, far closer to that of breast milk than to that of bovine-based formula. It has just two missing elements – antibodies (these are made by different cell types in the body) and the opportunity for microbial transfer from mother to baby.
Regardless, if something more closely resembling human milk can eventually be mass produced this would herald a new era in infant feeding. There are, of course, many hurdles left to jump before this idea becomes a reality. Both Biomilq and TurtleTree admit it will be a number of years before cell-cultured human milk in ready for mass production.
Significant challenges that lie ahead include identifying and sourcing the best cell type, scaling-up the manufacturing process, gaining regulatory approval for what is a very novel product and figuring out how to produce the milk for the same ballpark price as bovine formula.
Parents who formula-feed are likely to continue warmly welcoming the further humanisation of infant formulas – whether through the addition of HMOs, human-like proteins or the creation of a near-real-deal grown in the lab. However, support for these products is far from universal. It is feared that better formula feeding options may entice more parents not to breastfeed – something that all doctors and public health experts agree would be harmful. Such an unintended consequence is a valid concern but should it hinder infant formula innovation when, according to the WHO, only 40% of infants under six months of age are exclusively breastfed globally? That is one of those conundrums for which chemistry has no easy answer.
Nina Notman is a science writer based in Salisbury, UK
Update 16 Nov 2021: The structure of lacto-N-tetraose was corrected











3 readers' comments